Answer to Let in the Clowns
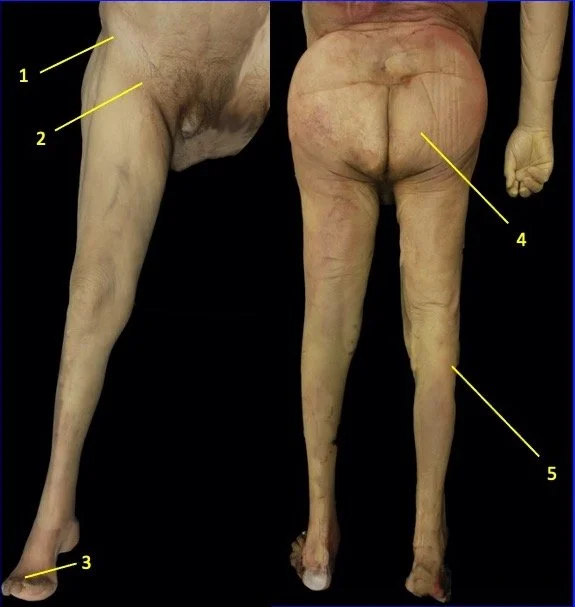
Correct answer is B. Blunt force to Point 1 is associated with the injury known as a “hip pointer”. Loss of sensation to area 3 is due to injuries of the deep fibular nerve. It becomes cutaneous at this region. Injuries to loss of sensation at this point can be due to injuring the common fibular nerve at Point 5. Injury to Point 4 would lead to sciatic nerve damage and most likely would also entail motor insufficiency, not just loss of sensation.
Based on the described scenario, the clown most likely received blunt goring to his inguinal area, the location of the femoral nerve and its branches, one of which is the medial cutaneous nerve of the leg (saphenous nerve). This nerve emerges superficially at the knee where the femoral artery dives deep to become the popliteal artery. The nerve then proceeds with the great saphenous vein to provide somatic sensory to the medial leg and the area just anterior to medial malleolus. While likely unlikely that only somatic sensory loss would have been experienced by such an injury, the described sensory deficit is only consistent with injury at location 2.
As a historical note, prior to central and PIC lines, the area just anterior to the medial malleolus was used to introduced catheters to patients who may be experiencing hypovolemic shock, for example, secondary to burns over large regions of their bodies (thorax and upper limbs). The procedure to insert a catheter into the great saphenous vein in this area was known as a cut-down. Prior to inserting the catheter, the saphenous nerve needed to be isolated to avoid injuring it by suturing the catheter in place. The establishment of venous access remains essential to the treatment and resuscitation of both the medically and traumatically ill patient. Adequate venous access allows the delivery of fluids, blood products, medications, and repeated blood sampling. This surgical procedure allows the clinician to gain venous access when relatively less invasive percutaneous procedures such as the Seldinger technique (percutaneous access), ultrasound-guided venous access, and intraosseous vascular access have failed. Percutaneous access can be difficult to achieve in certain patient populations (pediatric patients with small and nonpalpable veins, patients in hypovolemic shock with collapsed veins, patients with peripheral vascular disease with altered vascular anatomy) making venous cutdown a life-saving alternative.
Answer to this question is based on material presented in lecture 3 and 5 of the lower limb series.
Correct Answer is B.
A.1
B.2
C.3
D.4
E.5